Memory Loss — forgetfulness without impairment in function
Mild Cognitive Impairment (MCI) — more severe, defined as a MMSE 26-30
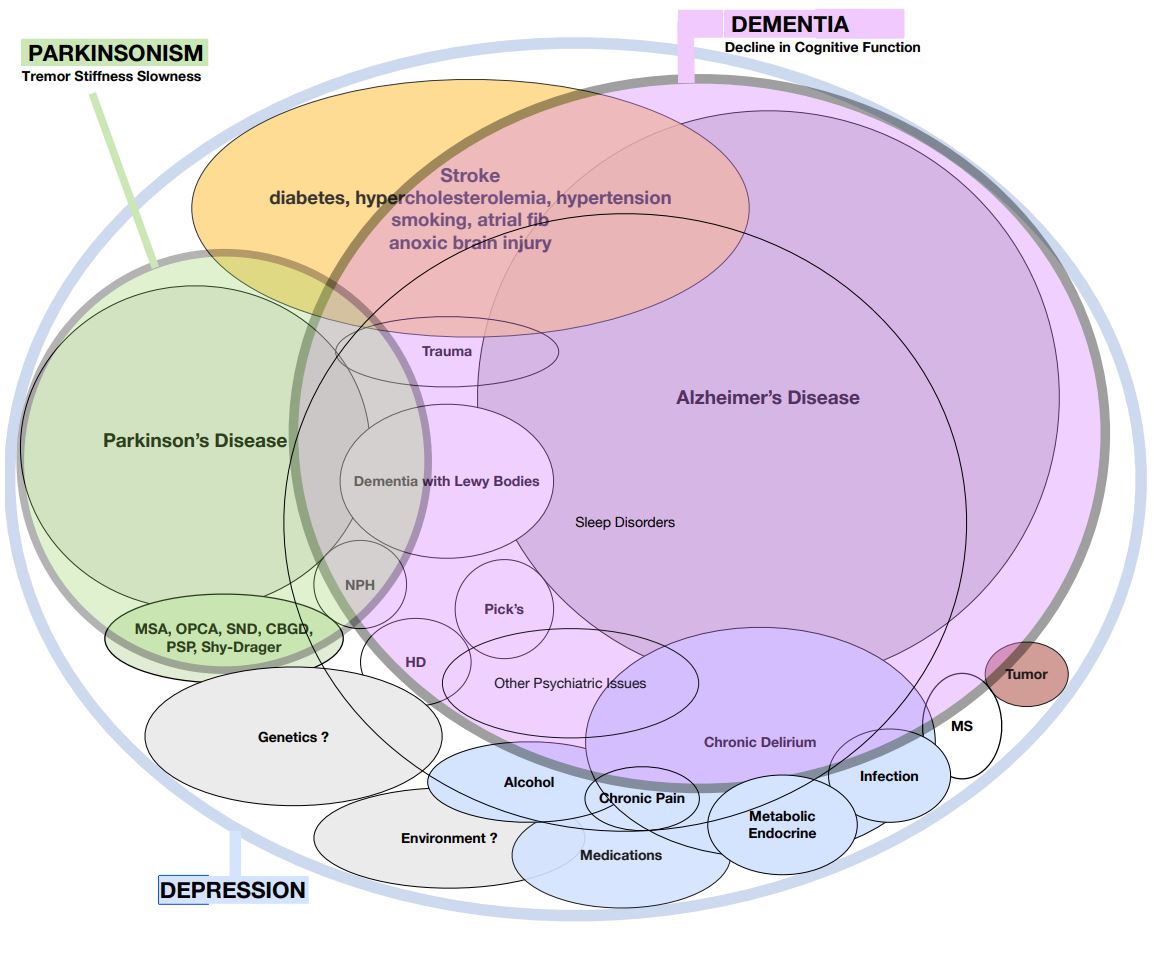
Dementia — a significant decline from a previous level of cognitive function which causes a significant impairment in social or occupational functioning.
Alzheimer’s disease is just one of the causes of dementia — the most common, but not the only.
- Age — Age remains the strongest risk factor for dementia, particularly for Alzheimer’s disease (AD) with rates as high as 50 percent of all people 85 years of age and
- Family History — People with a first-degree relative with AD have a 10 to 30 percent increased risk of developing the disorder overall; however, the increased risk is lower if your family member developed AD later in life (age 85 or older) and highest when the relatives were younger at age of onset Autosomal dominant inheritance of AD is rare (< 2% of all cases of AD). If it is “genetic” roughly half of all family members have dementia and affected family members usually develop symptoms prior to age 65.
- ApoE 4 — Everyone has inherited one ApoE from each parent so each of us has two of the three types — ApoE2, ApoE3 or ApoE4 — with “3/3” being most common in caucasians in the US. People who have two ApoE4s (they are “4/4”) are more likely to develop cardiovascular disease and dementia, but not guaranteed. So having one or two “4s” sounds scary but remember that ~40% of patients with AD do not have an ApoE 4 at all.
- Depression — Chronic depression, apathy and anxiety have all been linked to progressive cognitive decline, both in causation and as a reaction to the illness itself. There is no reason not to aggressively treat these concerns if present.
- Vascular disease — Risk factors commonly linked to heart attacks and stroke have also been linked to the development of dementia (including AD). These include, but are not limited to: Hyperlipidemia (high cholesterol), Hypertension (high blood pressure), Type II Diabetes (high blood sugars), Tobacco Smoking, Chronic Kidney Disease, Sleep Apnea, Dietary Fat and/or Obesity, and possibly Elevated Even if you are treated for these conditions (or you don’t know if you have them) signs of atherosclerosis on imaging tests (e.g. CT, MRI or carotid studies) are signs of increased risk as well.
- Lifestyle and Activity — Accumulating evidence suggests that three components of lifestyle – social, mental, and physical activity – are inversely associated with the risk for dementia — in other words, it’s good to socialize, be happy and exercise as they have all been shown to reduce your risk of dementia! Higher levels of education have also been associated with a reduced risk of AD so keep your brain active and around other people.
- Reversible causes
- Depression and Anxiety
- Delirium — sleep deprivation, chronic pain, etc. Metabolic or Endocrine disorders
- Nutritional deficiency or dehydration Hypoxia — tobacco, sleep apnea… Systemic illness — organ failure, infection…
- Lifestyle choices — little exercise, obesity, smoking…
- Toxicity — Alcohol, Medications, Poisons, Heavy Metals, Pesticides… Increased intracranial pressure — tumor, NPH, subdural hematoma…
- Brain Injury
- Trauma — traumatic brain injury (TBI) and chronic traumatic encephalopathy (CTE) Tumor (or paraneoplastic process)
- Infection / Encephalitis (viral, bacterial, fungal, AIDS, neuro-syphilis, anti-NMDA) Alcohol, lead, mercury, aluminum, carbon monoxide
- Stroke
- large vessels — vascular dementia or multi-infarct dementia small vessels — Binswanger’s encephalopathy
- cerebral amyloid
- angiopathy
- Neurodegeneration
- Alzheimer’s disease
- Primary Progressive Aphasia Posterior Cortical Atrophy
- Parkinsonism
- Parkinson’s disease
- Dementia with Lewy Bodies
- NPH
- PSP
- MSA
- SND
- OPCA
- CBD
- Fronto-temporal (Pick’s disease)
- Creutzfeld-Jakob disease
- Huntington’s disease
- Multiple Sclerosis
- Down syndrome
- Schizophrenia
History and Examination
- Braincheck®, PHQ-9
- MMSE or MoCA
- Neuropsychological testing (formal or “online”)
- EKG
- Overnight oximetry — consideration of sleep study if abnormal
Lab tests
The cost-effectiveness of obtaining multiple studies routinely in all patients is questioned because the yield is low. The prevalence of reversible dementia was < 1 percent in a 1994 study, and in another study in 2006, none of the 560 patients with dementia screened had a treatable cause of dementia identified.
- Standard
- CMP (electrolytes, kidney and liver function)
- TSH, CBC, B12, Folate (B9), Lipid panel
- Urinalysis
- Needs to be discussed prior to ordering
- PrecivityADTM — Aβ 42:40 ratio and ApoE
- HbA1c
- ESR +/- Auto-immune panel
- Vitamin D
- omega-3 index
- Rarely done
- urine tox screen, urine heavy metal screen, urinary free cortisol
- homocysteine, cortisol, testosterone, cystatin-C
- Vitamins B1, B3, B6
- For genetic testing: APP, Presenilin-1, Presenilin-2, Huntingtin gene
- CSF testing (lumbar puncture)
- Amyloid Βeta (Aβ42:Aβ40 ratio), total tau, p-tau181, p-tau217, GFAP, NfL
- opening pressure, cell count, protein, glucose
- Gram stain and culture
- Research only
- CSF 14-3-3, NSE, VLP1, MCP-1, YKL40
Radiology Tests
- MRI + volumetric analysis (basic MRI only finds something significant in 1 out of 180 scans)
- Metabolic FDG PET scan
- Amyloid PET scan — (sensitivity 89%-98%) (specificity to AD 88%-100%)
- Tau scan — (sensitivity 92%) (specificity to AD 80%)
Accident Prevention
— Falling is the #1 cause of injury, morbidity and mortality in people over the age of 65. A fall also leads to over 1.8 million emergency department visits, over 500,000 hospitalizations and over 16,000 deaths every year in the United States. Moreover, a head injury is a risk factor for dementia and can worsen a pre-existent dementia.
— Decide on an endpoint on when you will stop driving a car, not if.
Take care of your body
- Listen to your doctor
- Control blood pressure, blood cholesterol and blood sugars
- Limit medications and supplements — especially anti-cholinergic medications
- Limit alcohol
- No tobacco
- Maximize sleep and make it a priority
- Exercise! — 90 minutes of sustained aerobic exercise per week can reduce the development of dementia upwards of 60%! It doesn’t matter what exercise, just make it fun and just do it! e.g. juggling, T’ai Chi, walking, swimming…
Exercise your mind — and do it with other people! (brains like human interaction)
- Read / Engage / Enjoy / Volunteer (consider a book clubs, movie club, etc)
- Try a new activity or Experiment with new music, food, etc.
- Complex and/or Interactive Games (Scrabble®, Cribbage, ) are best
- Repetitive games done on your own are of questionable value (e.g. Sudoku)
- Be Happy, Content, Appreciative and Hopeful — Laugh and Be Social
- Counseling and Therapy, both individual and group It helps!
Improve your diet and hydration — consider supplements (if affordable)
- Limit fat, red meat and alcohol. Aim for a healthy weight for your
- Drink water — just do your best! — more if you’re dizzy or have dark urine
- Increase fruits and vegetables
- Vit B12, Folic acid, Vit C, Vit D 4000u, Vit E, zinc, omega-3 fatty acids (fish oil)
- ? coconut oil (1 Tbsp per day) vs Axona®
- ? L-serine
Brain Stimulation Devices
- light box therapy
- Vielight®
- TMS (Transcranial Magnetic Stimulation)
Plan Ahead
- Case management
- Long-term planning — “5 Wishes”
- Develop “5 Questions” to help family members make end-of-life decisions
Over-the-counter treatments are well-advertised but not well-studied. I can’t say that they hurt but have no good evidence to suggest that they do what is advertised.
FDA-approved prescriptions
- Acetylcholinesterase inhibitors — pills
- indicated for all stages of AD
- ~90% of people tolerate these medications but only ~ 50% see some benefit
- Aricept® / donepezil 5mg, 10mg, 23mg
- Exelon® / rivastigmine patch 4.6mg, 9.5mg, 13.3mg
- galantamine 8,16, 24 and ER
- NMDA receptor modulators — pills
- indicated for only moderate to late stage Alzheimer’s disease
- ~99% of people tolerate this drug
- Namenda® / memantine 10mg twice daily and 28mg XR
- Leqembi® — IV treatment every two weeks that removes Amyloid Plaque. It requires close monitoring including at least four MRIs in the first year. It is not for everyone with AD at all. We will only offer this product to selected patients after a careful review and screening process.
Biogen — aducanumab was FDA-approved in June 2021 but CMS/Medicare essentially stopped it from being commercially used. It is now back in Phase 3 research. It is a monoclonal antibody (like the recently FDA-approved Leqembi®) that removes amyloid plaque. We are actively enrolling patients for this study. https://clinicaltrials.gov/ct2/show/NCT05310071?term=aducanumab&draw=2&rank=7
WSU is actively enrolling patients for non-pharmaceutical studies. Contact Justin Frow, Laboratory Manager at WSU Neuropsychology and Aging Lab if interested. 509-335-4033
AriBio (mirodenafil) — AR1001 could be an effective treatment option with a mechanism of action that has not been explored for AD indication. We expect to be enrolling patients soon. https://clinicaltrials.gov/ct2/show/NCT05531526?term=ar1001&draw=2&rank=1
